Multiple antibiotic resistant index and detection of qnrS and qnrB genes in bacterial consortium of urine samples from clinical settings
Abstract
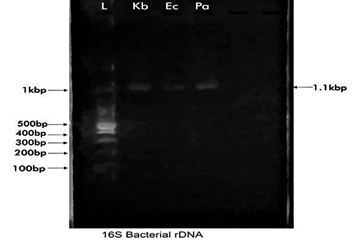
The multiple antibiotic resistant (MAR) index and detection of resistant genes in the bacterial consortium of urine samples collected from University of Medical Sciences Teaching Hospital, Akure (UNIMEDTH) was evaluated with all microbiological and biotechnological techniques employed utilizing specified standards in this study. Escherichia coli had the highest bacterial count (311.50 ± 0.707 CFU/ml) while Staphylococcus saprophyticus had the least (13.00 ± 2.828 CFU/ml). Enterococcus faecalis, and Pseudomonas aeruginosa isolate showed marked resistance against four classes of antibiotics tested. The MAR index of bacterial isolates ranged from 0.5 to 1.0. Fluoroquinolone-resistant P. aeruginosa identified to be P. aeruginosa via 16S rDNA analysis sequence analysis of 417 base pairs with strain mcbay1 deposited in GenBank with accession number MT423976 was positive for qnrS resistant gene. E. faecalis identified by 16S rRNA sequence analysis of 264 bp of the strain mcbay 2 deposited in GenBank with accession number MT423977 was also positive for qnrB resistant gene. The presence of resistant genes in ciprofloxacin-resistant P. aeruginosa and quinolone-resistant E. faecalis in urine samples further emphasized the need for the regulation of over-the-counter prescription and antibiotic susceptibility survey of anti-pseudomonal and anti-enterococcal quinolones in hospital settings.
Downloads
References
2. Jernberg C, Löfmark S, Edlund C, Jansson JK. Long-term ecological impacts of antibiotic administration on the human intestinal microbiota. Int Soc Microbial Ecol J. 2007; 1: 56-66.
3. Finley RL, Collignon P, Larsson DG, McEwen SA, Li WX, et al. The Scourge of Antibiotic Resistance: The Important Role of the Environment. Clin Infect Dis. 2013; 57(5): 704-710.
4. Poirel L, Cattoir V, Nordmann P, Plasmid-mediated quinolone resistance: interactions between human, animal and environmental ecologies. Front Microbiol. 2012; 3: 24.
5. Gillings MR, Stokes HW. Are humans increasing bacterial evolvability? Trends Ecol Evol. 2012; 6: 346-352.
6. Von Wintersdorff CJH, Penders J, VanNiekerk JM, Mills ND, Majumder S, et al. Dissemination of antimicrobial resistance in microbial ecosystems through horizontal gene transfer. Front Microbiol. 2016; 7(2): 173.
7. Etebu E, Arikekpar I. Antibiotics: Classification and mechanisms of action with emphasis on molecular perspectives. Int J Appl Microbiol Biotechnol Res. 2016; 4: 90-101.
8. Gillings MR. Lateral gene transfer, bacterial genome evolution, and the Anthropocene. Ann New York Acad Sci. 2017; 1389: 20-36.
9. Bekele T, Tesfaye A, Sewunet T, Waktola HD. Pseudomonas aeruginosa isolates and their antimicrobial susceptibility pattern among catheterized patients at Jimma University Teaching Hospital, Jimma, Ethiopia. BMC Res Notes. 2015; 8: 488.
10. Miller WR, Munita, JM, Arias CA. Mechanisms of antibiotic resistance in enterococci. Expert Rev Anti-Infect Ther. 2014; 12: 1221-1236.
11. Weng PL, Ramli R, Shamsudin MN, Cheah YK, Hamat RA. High genetic diversity of Enterococcus faecium and Enterococcus faecalis clinical isolates by pulsed-field gel electrophoresis and multi-locus sequence typing from a hospital in Malaysia. Biomed Res Int. 2013; 6: 23-29.
12. Geoffrey AO, Scolastica CK, Joan CC, Ongechi DR. Isolation, identification and characterization of urinary tract infectious bacteria and the effect of different antibiotics. J Nat Sci Res. 2013; 3(6): 150-159.
13. Atlas MR. Handbook of media for environmental microbiology. 2nd edn. Taylor & Francis publisher. NY. 2005; 33-43.
14. Hemraj V, Diksha S, Avneet, G. A review of commonly used biochemical test for bacteria. Inn J Life Sci. 2013; 1(1): 1-7.
15. Clinical Laboratory Standard Institute (CLSI), Performance Standards for antimicrobial susceptibity tests. Document M100-517. CLSI, Wagne, PA. Clin Microbiol. 2017; 45(1): 199-205.
16. Olsvik O, Strockbin NA. PCR detection of heat-stable, heat-label and shiga-like toxin genes in Escherichia coli. In: Persing DH, Smith TF., Tenover FC, White TJ. Diagnostic Molecular Microbiology. 9th edn. Am. Soc. for Microbiology. Washington, DC. 1993.
17. Robicsek A, Jacoby GA, Hooper DC. The worldwide emergence of plasmid-mediated quinolone resistance. Lancet Infect Dis. 2006; 6: 629-640.
18. Oyamada Y, Ito H, Inoue M, Yamagishi JI. Topoisomerase mutations and efflux are associated with fluoroquinolone resistance in Enterococcus faecalis. J Med Microbiol. 2006; 55(10): 1395-1401.
19. Kim HB, Park CH, Kim CJ, Kim EC, Jacoby GA, et al. Preva¬lence of plasmid-mediated quinolone resistance determi-nants over a 9-year period. Antimicrob Agents Chemother. 2009; 53(2): 639-645.
20. Chroma M, Kolar M. Genetic methods for detection of an¬tibiotic resistance: focus on extended-spectrum beta-lactamases. Biomed Pap Med Fac Univ Palacky Olomouc Czech Rep. 2010; 154(4): 289-296.
21. Huang B, Zhang L, Zhang W, Liao K, Zhang K, et al. Direct detection and identification of bacterial pathogens from urine with optimized specimen processing and enhanced testing algorithm. J Clin Microbiol. 2017; 55(5): 1488-1495.
22. Amin M, Mehdinejad M, Pourdangchi Z. Study of bacteria isolated from urinary tract infections and determination of their susceptibility to antibiotics. Jundishapur J Microbiol. 2009; 2(3): 118-128.
23. Shashwati N, Kiren T, Dhanvijay AG. Study of extended spectrum beta-lactamase producing Enterobacteriaceae and antibiotic co-resistance in a Tertiary Care Teaching Hospital. J Nat Sci Biol Med. 2014; 5(1): 30-35.
24. Mirsoleymani SR, Salimi M, Shareghi BM, Ranjbar M, Mehtarpoor M. Bacterial pathogens and antimicrobial resistance patterns in pediatric urinary tract infections: a four-year surveillance study (2009-2012). Int J Pediatrics. 2014; 2014: 126142.
25. Leski TA, Taitt CR, Bangura U, Stockelman MG, Ansumana R, et al. High prevalence of multidrug resistant Enterobacteriaceae isolated from outpatient urine samples but not the hospital environment in Bo, Sierra Leone. BMC Infect Dis. 2016; 16: 167.
26. Segar L, Kumar S, Joseph NM, Sivaraman UD. Prevalence of extended spectrum B-lactamases among Enterobacteriaceae and their antibiogram pattern from various clinical samples. Asian Pharm Clin Res. 2015; 8: 220-223.
27. Parajuli NP, Maharjan P, Joshi G, Khanal PR. Emerging perils of extended-spectrum lactamase producing Enterobacteriaceae clinical isolates in a Teaching Hospital of Nepal. BioMed Res Int. 2016; 2016: 1782835.
28. Livermore DM. Current epidemiology and growing resistance of gram negative pathogens. Korean J Int Med. 2012; 27: 128-142.
29. Andy IE, Okpo EA. Plasmid profile analysis and curing of multidrug resistant bacteria isolated from hospitals waste dumpsite in Calabar metropolis, Nigeria. Eur J Pharm Med Res. 2019; 6(5): 54-61.
30. Mohammed FA, Kadhim AK, Afraa AK, Ahmad AYK, Ciprofloxacin-resistance in Staphylococcus aureus and Pseudomonas aeruginosa isolated from Baghad. Int J Pharm Sci Res. 2015; 6(2): 302-385.
31. Najafi Mosleh M, Nasaj M, Rahimi F, Arabestani MR. Distribution rates and antibiotic resistance pattern of Enterococcus spp. isolated from clinical specimens of hospitals in hamedan. J Mazandaran Univ Med Sci. 2014; 24: 92-102.
32. Fozouni L, Askari H, Pordeli HR. Frequency distribution of fluoroquinolones-resistant Enterococcus faecalis isolates from patients with prostatitis in Golestan Province. Iran Med Lab J. 2019; 13: 29-33.
33. Datta P, Thakur A, Mishra B, Gupta V. Prevalence of clinical strains resistant to various beta-lactams in a tertiary care hospital in India. Jap J Infect Dis. 2004; 57(4): 146-149.

This work is licensed under a Creative Commons Attribution 4.0 International License.