In silico molecular docking of selected polyphenols against interleukin-17A target in gouty arthritis
Abstract
The binding of Interleukin-17A (IL-17A) to its receptor causes the release of chemokine which have an implication in the pathogenesis of gouty arthritis. Though, some synthetic drugs have been proved worthy as IL-17A inhibitors in the management of gout but they have been associated with a number of side effects. Polyphenols have been documented for numerous therapeutic applications. In spite of this, there are scarce data on the mechanism of action and protective potentials of polyphenolic against gouty arthritis. This present in silico study aimed to assess the inhibitory potentials and ADMET properties of selected polyphenols against IL-17A using molecular docking tools. The crystal structure of IL-17A was retrieved from the protein database, while the structures of polyphenolic compounds were retrieved from Pubchem. Drug-likeness of the polyphenols was assessed using DruLiTo. A total of 22 out of 26 polyphenols investigated passed the Lipinski drug likeness rule of five which were then docked with the active site of IL-17A using docking software, and the docked complexes were analyzed using LigPlot and protein-ligand profiler web server. The results showed that all the investigated polyphenols have appreciable higher binding affinity when compared to the standard drug (allopurinol) with pelargondin and catechin having the highest binding affinity (-7.5 kcal/mol). Furthermore, ADMET screening were carried out on the five compounds with the best hits. Conclusively, this in silico study suggests that these investigated polyphenols could serve as better replacements for synthetic drugs such as allopurinol in the management of gouty arthritis.
Downloads
References
2. Saigal R, Agrawal A. Pathogenesis and clinical management of gouty arthritis. J Assoc Physicians India. 2015; 63: 56-63.
3. Ragab G, Elshahaly M, Bardin T. Gout: an old disease in new perspective - a review. J Adv Res. 2017; 8(5): 495-511.
4. Doherty M. New insights into the epidemiology of gout. Rheumatology. 2009; 48: ii2-8.
5. Chiu CC, Chen CH, Huang MC, Chen PY, Tsai CJ, Lu ML. The relationship between serum uric acid concentration and metabolic syndrome in patients with schizophrenia or schizoaffective disorder. J Clin Psychopharmacol. 2012; 32(5): 585-592.
6. Feig DI, Kang DH, Johnson RJ. Uric acid and cardiovascular risk. N Engl J Med. 2008; 359(17): 1811-1121.
7. Grayson PC, Kim SY, LaValley M, Choi HK. Hyperuricemia and incident hypertension: a systematic review and meta-analysis. Arthritis Care Res. 2011; 63(1): 102-110.
8. Mohandas R, Johnson RJ. Uric acid levels increase risk for new-onset kidney disease. J Am Soc Nephrol. 2008; 19(12): 2251-2253.
9. Soltani Z, Rasheed K, Kapusta DR, Reisin E. Potential role of uric acid in metabolic syndrome, hypertension, kidney injury, and cardiovascular diseases: is it time for reappraisal? Curr Hypertens Rep. 2013; 15(3): 175-181.
10. Kostalova E, Pavelka K, Vlaskova H, Musalkova D, Stiburkova B. Hyperuricemia and gout due to deficiency of hypoxanthine-guanine phosphoribosyltransferase in female carriers: new insight to differential diagnosis. Clin Chim Acta. 2015; 440: 214-217.
11. Raucci F, Iqbal AJ, Saviano A, Minosic P, Piccolo M, Irace C, et al. IL-17A neutralizing antibody regulates monosodium urate crystal-induced gouty inflammation. Pharmacol Res. 2019; 147: 104351.
12. El Ridi R, Tallima H. Physiological functions and pathogenic potential of uric acid: a review. J Adv Res. 2017; 8(5): 487-493.
13. Roddy E, Doherty M. Epidemiology of gout. Arthritis Res Ther. 2010; 12(223): 1-11.
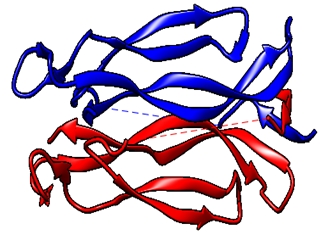
14. Liu S, Song X, Chrunyk BA, Shanker S, Hoth LR, et al. Crystal structures of interleukin 17A and its complex with IL-17 receptor A. Nat Commun. 2013; 4: 1888.
15. Chang SH, Reynolds JM, Pappu BP, Chen G, Martinez GJ, Dong C. Interleukin-17C promotes Th17 cell responses and autoimmune disease via interleukin-17 receptor E. Immunity. 2011; 35: 611-621.
16. Gaffen SL, Hernandez-Santos N, Peterson AC. IL-17 signaling in host defense against Candida albicans. Immunol Res. 2011; 50: 181-187.
17. Gaffen, SL. Structure and signaling in the IL-17 receptor family. Nat Rev Immunol. 2009; 9: 556-567.
18. Kramer JM, Gaffen SL. Interleukin-17: a new paradigm in inflammation, autoimmunity and therapy. J Periodontol. 2007; 78: 1083-1093.
19. Miossec P. Update on interleukin-17: a role in the pathogenesis of inflammatory arthritis and implication for clinical practice. RMD Open. 2017; 3: e000284.
20. Kirkham BW, Kavanaugh A, Reich K. Interleukin-17A: a unique pathway in immune-mediated diseases: psoriasis, psoriatic arthritis and rheumatoid arthritis. Immunology. 2014; 141(2): 133-142.
21. Zhang X, Angkasekwinai P, Dong C, Tang H. Structure and function of interleukin-17 family cytokines. Protein Cell. 2011; 2(1): 26-40.
22. Cavalcanti NG, Marques CD, Lin’s e Lins TU, Pereira MC, Rêgo MJ, Duarte AL, et al. Cytokine profile in gout: inflammation driven by IL-6 and IL-18? Immunol Invest. 2016; 45(5): 383-395.
23. Gaffen SL. The role of interleukin-17 in the pathogenesis of rheumatoid arthritis. Curr Rheumatol Rep. 2009; 11: 365e370.
24. Kwan BC, Tam LS, Lai KB, Lai FM, Li EK, Wang G, et al. The gene expression of type 17 T-helper cell-related cytokines in the urinary sediment of patients with systemic lupus erythematosus. Rheumatology. 2009; 48: 1491e1497.
25. Liu Y, Zhao Q, Yin Y, McNutt MA, Zhang T, Cao Y Serum levels of IL-17 are elevated in patients with acute gouty arthritis. Biochem Biophys Res Comm. 2018; 497: 897e902.
26. Schwab N, Zozulya AL, Kieseier BC, Toyka KV, Wiendl H. An imbalance of two functionally and phenotypically different subsets of plasmacytoid dendritic cells characterizes the dysfunctional immune regulation in multiple sclerosis. J Immunol. 2010; 184: 5368e5374.
27. Yu H, Huang J, Liu Y, Ai G, Yan W, Wang X, Ning Q. IL-17 contributes to autoimmune hepatitis. J Huazhong Uni. Sci Technol Med Sci. 2010; 30: 443e446.
28. Le Goff B, Bouvard B, Lequerre T, Lespessailles E, Marotte H, Pers YM, Cortet B. Implication of IL-17 in bone loss and structural damage in inflammatory rheumatic diseases. Mediat Inflam. 2019: 8659302.
29. Kuwabara T, Ishikawa F, Kondo M, Kakiuchi T. The role of IL-17 and related cytokines in inflammatory autoimmune diseases. Mediat Inflam. 2017: 3908061.
30. Van Den Berg WB, Miossec P. IL-17 as a future therapeutic target for rheumatoid arthritis. Nat Rev Rheumatol. 2009; 5: 549e553.
31. Zhou Z, Li X, Li H, Guo M, Liu S, Li C. Genetic analysis of IL- 17 gene polymorphisms in gout in a male Chinese Han population. PLoS One. 2016; 11(2): e0148082.
32. Verma S. Medicinal plants with anti-inflammatory activity. J Phytopharmacol. 2016; 5(4): 157-159.
33. Panda SK, Thatoi HN, Dutta SK. Antibacterial activity and phytochemical screening of leaf and bark extracts of Vitex negundo from Similipal biosphere reserve Orissa. J Med Plant Res. 2009; 3(4): 294-300.
34. Sobhani M, Farzaei MH, Kiani S, Khodarahmi R. Immunomodulatory; anti-inflammatory/antioxidant effects of polyphenols: a comparative review on the parental compounds and their metabolites. Food Rev Int. 2020; doi: 10.1080/87559129.2020.1717523.
35. Oliviero F, Scanu A, Zamudio-Cuevas Y, Punzi L, Spinella P. Anti-inflammatory effects of polyphenols in arthritis. J Sci Food Agric. 2017; 98(5): 1653-1659.
36. Gliozzi M, Malara N, Muscoli S, Mollace V. Review on the treatment of hyperuricemia. Int J Cardiol. 2016; 213: 23-27.
37. Pacher P. Therapeutic effects of xanthine oxidase inhibitors: renaissance half a century after the discovery of allopurinol. Pharmacol Rev. 2006; 58(1): 87-114.
38. Stamp LK, O'Donnell JL, Zhang M, James J, Frampton C, Barclay ML, et al. Using allopurinol above the dose based on creatinine clearance is effective and safe in patients with chronic gout, including those with renal impairment. Arthritis Rheum. 2011; 63: 412-421.
39. Thabitha A, Mohamed Thoufic Ali AM, Singh SK, Rakhi, Varsha S, Mohana PA, Sajitha LS. Targeting IL-17 AND IL-17D receptors of rheumatoid arthritis using phytocompounds: A molecular docking study. IOP Conf Series Materials Sci Engin. 2017; 263: 022040.
40. Pettersen EF, Goddard TD, Huang CC, Couch GS, Greenblatt DM, Meng EC, Ferrin TE. UCSF Chimera - A visualization system for exploratory research and analysis. J Comput Chem. 2004; 25(13): 1605-1612.
41. Volkamer A, Kuhn D, Grombacher T, Rippmann F, Rarey, M. Combining global and local measures for structure-based druggability predictions. J Chem Inform Model. 2012; 52: 360-372.
42. Lipinski CA, Lombardo F, Dominy BW, Feeney PJ. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv Drug Delivery Rev. 2001; 46: 3-26.
43. Lipinski CA. Drug-like properties and the causes of poor solubility and poor permeability. J Pharm Toxicol Methods. 2008; 44: 235-249.
44. Trott O, Olson AJ. AutoDock Vina: improving the speed and accuracy of docking with a new scoring function, efficient optimization, and multithreading. J Comput Chem. 2010; 31: 455-461.
45. Kamaz Z, Al-jassani MJ, Umar HI. Screening of common herbal medicines as promising direct inhibitors of Sars-Cov-2 in silico. Annu Res Rev Biol. 2020; 35(8): 53-67.
46. Daina A, Michielin O, Zoete V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Scient Rep. 2017; 7: 1-13.
47. Cheng F, Li W, Zhou Y, Jie S, Wu Z, et al. AdmetSAR: a comprehensive source and free tool for assessment of chemical ADMET properties. J Chem Inform Model. 2012; 2: 3099-3105.
48. Yang H, Lou C, Sun L, Li J, Cai Y, et al. AdmetSAR 2.0 : web-service for prediction and optimization of chemical ADMET properties. Bioinformatics. 2018; doi: 10.1093/bioinformatics/bty707/5085368
49. Mannangatti P, Naidu, KN. Indian herbs for the treatment of neurodegenerative disease. Adv Neurobiol. 2016; 12: 323-336.
50. Ernst M, Grace OM, Saslis-Lagoudakis CH, Nilsson N, Simonsen HT, Ronsted N. Global medicinal uses of Euphorbia L. (Euphorbiaceae). J Ethnopharmacol. 2015; 176: 90-101.
51. Gozubuyuk GS, Aktas E, Yigit N. An ancient plant Lawsonia inermis (henna): Determination of in vitro antifungal activity against dermatophytes species. J Mycol Med. 2014; 24: 313-318.
52. Hotwani K., Baliga S, Sharma K. Phytodentistry: Use of medicinal plants. J Complem Integr Med. 2014; 11: 233-251.
53. Liu Q, Lawrence AJ, Liang JH. Traditional Chinese medicine for treatment of alcoholism: From ancient to modern. Am J Chin Med. 2011; 39: 1-13.
54. McGovern PE, Mirzoian A, Hall GR. Ancient Egyptian herbal wines. Proc Natl Acad Sci USA. 2009; 106: 7361-7366.
55. Thomford NE, Senthebane DA, Rowe A, Munro D, Seele P, et al. Natural products for drug discovery in the 21stcentury: innovations for novel drug discovery. Int J Mol Sci. 2018; 19: 1578.
56. Usha T, Middha SK, Goyal AK, Karthik M, Manoj DA, et al. Molecular docking studies of anti-cancerous candidates in Hippophae rhamnoides and Hippophae salicifolia. J Biomed Res. 2014; 28(5): 406-415.
57. Singh SP, Konwar BK. Molecular docking studies of quercetin and its analogues against human inducible nitric oxide synthase. SpringerPlus. 2012; 1: 69.
58. Kolls JK, Linden A. interleukin-17 family members and inflammation. Immunity. 2004; 21(4): 467-476.
59. Stojanovi DS, Zari D. Hydrogen bonds and hydrophobic interactions of porphyrins in porphyrin-containing proteins. Open Struct Biol J. 2009; 3: 34-41.
60. Ogunwa TH, Ayenitaju FC. Molecular binding signatures of morelloflavone and its naturally occurring derivatives on HMG-COA reductase. Int J Biol Sci Applic. 2017; 4(5): 74-81.
61. Mohapatra S, Prasad A, Haque F, Ray S, De B, Ray SS. In silico investigation of black tea components on α-amylase, α-glucosidase and lipase. J Appl Pharm Sci. 2015; 5(12): 42-47.
62. Muir SW, Harrow C, Dawson J, Lees KR, Weir CJ, Sattar N, Walters MR. Allopurinol use yields potentially beneficial effects on inflammatory indices in those with recent ischemic stroke: a randomized, double-blind, placebo-controlled trial. Stroke. 2008; 39(12): 3303-3307.
63. Jeong S, Ku SK, Bae JS. Anti-inflammatory effects of pelargonidin on TGFBIp-induced responses. Can J Physiol Pharmacol. 2017; 95(4): 372-381.
64. Kang H, Lee T, Bae JS. Suppressive effects of pelargonidin on endothelial protein C receptor shedding via the inhibition of TACE activity and MAP kinases. Am J Chin Med. 2016; 44(4): 771-784.
65. Fan FY, Sang LX, Jiang M. Catechins and their therapeutic benefits to inflammatory bowel disease. Molecules. 2017; 22(3): 484.
66. Oldoni TLC, Melo PS, Massarioli, AP, Moreno IAM, Bezerra RMN, et al. Bioassay-guided isolation of proanthocyanidins with antioxidant activity from peanut (Arachis hypogaea) skin by combination of chromatography techniques. Food Chem. 2016; 192: 306-312.
67. Li Y, Yao J, Han C, Yang J, Chaudhry MT. Quercetin, inflammation and immunity. Nutrients. 2016; 8(3): 167.
68. Wang H, Cao ZR. Anti-inflammatory effects of (-)-Epicatechin in lipopolysaccharide-stimulated raw 264.7 macrophages. Trop J Pharm Res. 2014; 13(9): 1415.
69. Wang J, Fang X, Ge L, Cao F, Zhao L, Wang Z, Xiao W. Antitumor, antioxidant and anti-inflammatory activities of kaempferol and its corresponding glycosides and the enzymatic preparation of kaempferol. PLoS One. 2018; 13(5): e0197563.
70. Manchope MF, Calixto-Campos C, Coelho-Silva L, Zarpelon AC, Pinho-Ribeiro FA, Georgetti SR, et al. Naringenin inhibits superoxide anion-induced inflammatory pain: role of oxidative stress, cytokines, Nrf-2 and the NO-cGMP-PKG-KATP channel signaling pathway. PLoS One. 2016; 11: e0153015.
71. Manchope MF, Casagrande R, Verri, Jr WA. Naringenin: an analgesic and anti-inflammatory citrus flavanone. Oncotarget. 2017; 8(3): 3766-3767.
72. Hostetler GL, Ralston RA, Schwartz SJ. Flavones: Food sources, bioavailability, metabolism, and bioactivity. Adv Nutr. 2017; 8: 423-435.
73. Fidelis QC, Faraone I, Russo D, Aragão Catunda FE Jr., Vignola L, et al. Chemical and biological insights of Ouratea hexasperma (A. St.-Hil.) Baill: A source of bioactive compounds with multifunctional properties. Nat Prod Res. 2014; 2018: 1-4.
74. Villa-Rodriguez JA, Kerimi A, Abranko L, Tumova S, Ford L, et al. Acute metabolic actions of the major polyphenols in chamomile: An in vitro mechanistic study on their potential to attenuate postprandial hyperglycaemia. Sci Rep. 2018; 3: 5471.
75. Lim R, Barker G, Wall CA, Lappas M. Dietary phytophenols curcumin, naringenin and apigenin reduce infection-induced inflammatory and contractile pathways in human placenta, foetal membranes and myometrium. Mol Hum Reprod. 2013; 19: 451-462.
76. Zhou Z, Zhang Y, Lin L, Zhou J. Apigenin suppresses the apoptosis of H9C2 rat cardiomyocytes subjected to myocardial ischemia-reperfusion injury via up regulation of the PI3K/Akt pathway. Mol Med Rep. 2018; 18: 1560-1570.
77. Aggarwal BB, Kumar A, Bharti AC. Anticancer potential of curcumin: Preclinical and clinical studies. Anticancer Res. 2003; 23: 363-398.
78. Mahmoud AM, Hernández-Bautista RJ, Sandhu MA, Hussein OE. Beneficial effects of citrus flavonoids on cardiovascular and metabolic health. Oxid Med Cell Longev. 2019; 19: ID 5484138.
79. Samie R, Sedaghat T, Baluchnejadmojarad T, Roghani M. Hesperetin, a citrus flavonoid, attenuates testicular damage in diabetic rats via inhibition of oxidative stress, inflammation, and apoptosis. Life Sci. 2018; 210: 132-139.

This work is licensed under a Creative Commons Attribution 4.0 International License.