The first report of the coproduction of CMY-16 and ArmA 16S rRNA methylases in carbapenemase-ESBL producing Escherichia coli isolates
Abstract
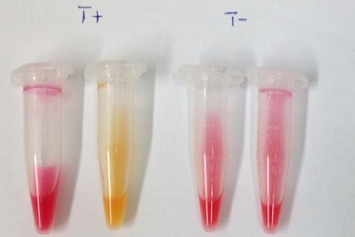
The main aim of this work was to assess the occurrence and to characterize AmpC genes and to investigate the co-existence of 16S rRNA methylases and carbapenemases genes among the ESBL producing Escherichia coli strains. 180 Escherichia coli clinical strains were collected from the university hospital of Constantine located in the eastern part of Algeria. 42 ESBL-producers were phenotypically identified and also confirmed genotypically able to produce CTX-M-15 [n=33], CTX-M-1 [n=5], CTX-M-14 [n=1], SHV-2 [n=1], and two strains have been revealed producing the blaOXA-48 genes associated with blaTEM-1. Among the ESBL-producing strains three expressed additionally an AmpC phenotype which corresponded to the carriage of a blaCMY gene shown by sequencing to correspond to CMY-2 (1 isolate) CMY-16 (2 isolates). The two E. coli isolates produce CMY-16 that belonged to phylogroup D while the single CMY-2 producing isolate belonged to phylogroup C. Antibiotic resistance of the aminoglycoside family by production of 16S rRNA methylases was detected by an end-point multiplex PCR assay which concerns genes coding for different 16S rRNA methylases (rmtD, rmtA, rmtB, armA, npmA, and rmtC). An armA gene was identified in 2 strains. This study shows for the first time the co-existance of CMY-16 and armA genes with blaTEM-1 and blaOXA-48 producing E. coli strains.
Downloads
References
2. Branger C, Zamfir O, Geoffroy S, Laurans G, Arlet G, Thien HV, et al. Genetic background of Escherichia coli and extended-spectrum beta-lactamase type. Emerg Infect Dis. 2005; 11(1): 54-61.
3. Krishnappa LG, John J, Marie MAM, Gopalkrishnan S, Pradeep CS, Rani SRB. Detection of pan-amino glycoside-resistant Gram negative bacteria using a molecular method. South Asian J Exp Biol. 2012; 2: 256–8.
4. Sahni RD, Balaji V, Varghese R, John J, Tansarli GS, Falagas ME. Evaluation of fosfomycin activity against uropathogens in a fosfomycin-naive population in South India: a prospective study. Future Microbiol. 2013; 8: 675-680.
5. Agabou A, Pantel A, Ouchenane Z, Lezzar N, Khemissi S, Satta D, et al. First description of OXA-48-producing Escherichia coli and the pandemic clone ST131 from patients hospitalized at a military hospital in Algeria. Eur J Clin Microbiol Infect Dis. 2014; 33: 1641-1646.
6. Mammina C, Di Carlo P, Cipolla D, Giuffrè M, Casuccio A, Di Gaetano V, et al. Surveillance of multidrug-resistant gram-negative bacilli in a neonatal intensive care unit: prominent role of cross transmission. Am J Infect Control. 2007; 35: 222-230.
7. Philippon A, Arlet G, Jacoby GA. Plasmid-mediated AmpC-type-lactamases. Antimicrob Agents Chemother. 2002; 46: 1-11.
8. Perez-Perez FJ, Hanson ND. Detection of plasmid-mediated AmpC betalactamase genes in clinical isolates by using multiplex PCR. J Clin Microbiol. 2002; 40: 2153-2162
9. Iabadene H, Messai Y, Ammari H, Alouache S, Verdet C, Bakour R, Arlet G. Prevalence of plasmid-mediated AmpC-lactamases among Enterobacteriaceae in Algiers hospitals. Int J Antimicrob Agents. 2009; 34: 340-342.
10. Yim G, Kwong W, Davies J, Miao V. Complex integrons containing qnrB4-ampC (blaDHA-1) in plasmids of multidrug-resistant Citrobacter freundii from wastewater. Can J Microbiol. 2013; 59: 110-116.
11. Lee H, Yong D, Yum JH, Roh KH, Lee K, Yamane K, et al. Dissemination of 16S rRNA methylase-mediated highly amikacin-resistant isolates of Klebsiella pneumoniae and Acinetobacter baumannii in Korea. Diagn Microbiol Infect Dis 2006; 56: 305-312.
12. Doi Y, Yokoyama K, Yamane K, Wachino J-I, Shibata N, Yagi T, et al. Plasmid-mediated 16S rRNA methylase in Serratia marcescens conferring high-level resistance to aminoglycosides. Antimicrob Agents Chemother. 2004; 48: 491-496.
13. Galimand M, Courvalin P, Lambert T. Plasmid-mediated high-level resistance to aminoglycosides in Enterobacteriaceae due to 16S rRNA methylation. Antimicrob Agents Chemother. 2003; 47: 2565-2571.
14. Hidalgo L, Hopkins KL, Gutierrez B, Ovejero CM, Shukla S, Douthwaite S, et al. Association of the novel aminoglycoside resistance determinant RmtF with NDM carbapenemase in Enterobacteriaceae isolated in India and the UK. J Antimicrob Chemother. 2013; 68: 1543-1550.
15. Yamane K, Wachino J, Suzuki S, Shibata N, Kato H, Shibayama K, et al. 16S rRNA methylase-producing, gram-negative pathogens, Japan. Emerg Infect Dis. 2007; 13: 642-646.
16. Bogaerts P, Galimand M, C Bauraing, Deplano A, Vanhoof R, De Mendonca R, et al. Emergence of ArmA and RmtB aminoglycoside resistance 16S rRNA methylases in Belgium. J Antimicrob Chemother. 2007; 59: 459-464.
17. Nordmann P, Poirel L, Dartet L. Rapid detection of carbapenemase-producing Enterobacteriaceae. Emerg Infect Dis. 2012; 18: 1503-1507.
18. Bakour S, Olaitan AO, Ammari H, Touati A, Saoudi S, Saoudi K, Rolain JM. Emergence of colistin- and carbapenem-resistant Acinetobacter baumannii ST2 clinical isolate in Algeria: first case report. Microb.Drug Resist. 2015; 21(3): 279-285.
19. Yong D, Lee K, Yum JH, Shin HB, Rossolini GM, Chong Y. Imipenem-EDTA disk method for differentiation of metallo-beta-lactamase-producing clinical isolates of Pseudomonas spp. and Acinetobacter spp. J Clin Microbiol. 2002; 40(10): 3798-3801.
20. Bogaerts P, Rezende de Castro R, De Mendonça R, Huang TD, Denis O, Glupczynski Y. Validation of carbapenemase and extended-spectrum beta-lactamase multiplex endpoint PCR assays according to ISO 15189. J Antimicrob Chemother. 2013; 68: 1576-1582.
21. Nicolas-Chanoine MH, Blanco J, Leflon-Guibout V, Demarty R, Alonso MP, Caniça MM, et al. Intercontinental emergence of Escherichia coli clones O25:H4-ST131 producing CTX-M-15. J Antimicrob Chemother. 2008; 61(2): 273-281.
22. Clermont O, Dhanji H, Upton M, Gibreel T, Fox A, Boyd D, et al. Rapid detection of the O25b-ST131 clone of Escherichia coli encompassing the CTX-M-15 producing strains. J Antimicrob Chemother. 2009; 64: 274-277.
23. Clermont O, Christenson JK, Denamur E, Gordon DM. The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of newphylo-groups. Environ Microbiol. 2013; 5: 58-65.
24. Baba Ahmed-Kazi Tani Z, Decré D, Genel N, Boucherit-Otmani Z, Arlet G, Drissi M. Molecular and epidemiological characterization of enterobacterial multidrug resistant strains in Tlemcen Hospital (Algeria) (2008-2010). Microb Drug Resist. 2013; 19: 185-190.
25. Girlich D, Bouihat N, Poirel L, Benouda A, Nordmann P. High rate of faecal carriage of extended-spectrum b-lactamase and OXA-48 carbapenemase producing Enterobacteriaceae at a University hospital in Morocco. Clin Microbiol Infect. 2014; 20: 350-354.
26. Rogers BA, Sidjabat HE, Paterson DL. Escherichia coli O25b-ST131: a pandemic, multiresistant, community-associated strain. J Antimicrob Chemother. 2011; 66(1): 1-14.
27. Ayad A, Drissi M, de Curraize C, Dupont C, Hartmann A, Solanas S, et al. Occurrence of ArmA and RmtB aminoglycoside resistance 16S rRNA methylases in extended-spectrum β-lactamases producing Escherichia coli in Algerian hospitals. Front Microbiol. 2016; 7: 1409.
28. Verdet C, Benzarara Y, Gautier V, Adam O, Ould-Hocine Z, Arlet G. Emergence of DHA-1 producing Klebsiella spp. in the Parisian region: genetic organization of the ampC and ampR genes originating from Morganella morganii. Antimicrob Agents Chemother. 2006; 50: 607-617.
29. Yilmaz NO, Agus N, Bozcal E, Oner O, Uzel A. Detection of plasmid-mediated AmpC beta-lactamase in Escherichia coli and Klebsiella pneumoniae. Indian J Med Microbiol. 2013; 31: 53-59.
30. Denisuik AJ, Lagacé-Wiens PR, Pitout JD, Mulvey MR, Simner PJ, Tailor F, et al. Molecular epidemiology of extended-spectrum beta-lactamase, AmpC beta-lactamase and carbapenemase producing Escherichia coli and Klebsiella pneumoniae isolated from Canadian hospitals over a 5 year period: CANWARD 2007-11. J Antimicrob Chemother. 2013; 68: 57-65.
31. Mnif B, Ktari S, Chaari A, Medhioub F, Rhimi F, Bouaziz M, Hammami A. Nosocomial dissemination of Providencia stuartii isolates carrying blaOXA-48, blaPER-1, blaCMY-4 and qnrA6 in a Tunisian hospital. J Antimicrob Chemother. 2013; 68: 329-332.
32. D’Andrea MM, Nucleo E, Luzzaro F, Giani T, Migliavacca R, Vailati F, et al. CMY-16, a novel acquired AmpC-type beta-lactamase of the CMY/LAT lineage in multifocal monophyletic isolates of Proteus mirabilis from northern Italy. Antimicrob Agents Chemother. 2006; 50: 618-624.
33. D’Andrea MM, Literacka E, Zioga A, Giani T, Baraniak A, Fiett J, et al. Evolution and spread of multidrug-resistant Proteus mirabilis clone with chromosomal AmpC β-lactamase in Europe. Antimicrob Agents Chemother. 2011; 55: 2735-2742.
34. Migliavacca R, Migliavacca A, Nucleo E, Ciaponi A, Spalla M, De Luca C, Pagani L. Molecular epidemiology of ESBL producing Proteus miraiblis isolates from a long –term care and rehabilitation facility in Italy. New Microbiol. 2007; 30: 362-366.
35. Bedenić B, Firis N, Elveđi-Gašparović V, Krilanović M, Matanović K, Štimac I, et al. Emergence of multidrug-resistant Proteus mirabilis in a longterm care facility in Croatia. Wiener Klin Wochenschrift. 2016; 128: 404-413.
36. Salome NS, Jonas M, Vincent P, Alessandra C, Hansjakob F, Andrea E. Emergence of Klebsiella pneumoniae co-producing NDM-1, OXA-48, CTX-M-15, CMY-16, QnrA and ArmA in Switzerland. Int J Antimicrob Agents. 2014; 44: 260-262.
37. Chérif T, Saidani M, Decré D, Boutiba-Ben Boubaker I, Arlet G. Cooccurrence of multiple AmpC-lactamases in Escherichia coli, Klebsiella pneumoniae, and Proteus mirabilis in Tunisia. Antimicrob Agents Chemother. 2016; 60: 44-51.