Detection of carbapenem resistant bacteria (CRB) in Egypt
Abstract
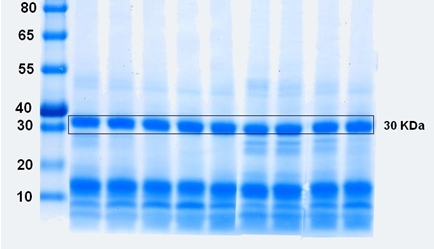
The emergence of resistant bacteria has become a worldwide threat. Multidrug resistant bacteria are globally spread. Several studies were performed to detect new resistant organisms and also the genes which are responsible for their resistance. Carbapenem resistance is considered the most dangerous resistance. In this study, we detect the presence of carbapenem resistant bacteria (CRB) in Egypt. This may cause un-treatable epidemic if its organization is neglected. This study distinguished the pathogens that are carbapenemase producing due to the presence of bla-NDM gene. The results detected the presence of CRB stains such as Klebsiella sp., Pseudomonas sp., Citrobacter sp., Enterobacter sp., Acinetobacter sp. and E. coli. As a result from this study, it is now proved that there are CRB in Egypt, thus it must be given a great consideration and must be managed.
Downloads
References
2. Richter SN, Frasson I, Franchin E, Bergo C, Lavezzo E, Barzon L, et al. KPC-mediated resistance in Klebsiella pneumoniae in two hospitals in Padua, Italy, June 2009-December 2011: massive spreading of a KPC-3-encoding plasmid and involvement of non-intensive care units. Gut Pathogens. 2012; 4(1): 7.
3. Drawz SM, Bonomo RA. Three decades of β-lactamase inhibitors. Clin Microbiol Rev. 2010; 23(1): 160-201.
4. Palzkill T. Metallo‐β‐lactamase structure and function. Ann New York Acad Sci. 2013; 1277(1): 91-104.
5. Bebrone C. Metallo-β-lactamases (classification, activity, genetic organization, structure, zinc coordination) and their superfamily. Biochem Pharmacol. 2007; 74(12): 1686-1701.
6. Bebrone C, Lassaux P, Vercheval L, Sohier J-S, Jehaes A, Sauvage E, et al. Current challenges in antimicrobial chemotherapy. Drugs. 2010; 70(6): 651-679.
7. Bush K. The ABCD’s of β-lactamase nomenclature. J Infect Chemother. 2013; 19(4): 549-559.
8. Tijet N, Boyd D, Patel SN, Mulvey MR, Melano RG. Evaluation of the Carba NP test for rapid detection of carbapenemase-producing Enterobacteriaceae and Pseudomonas aeruginosa. Antimicrob Agents Chemother. 2013; 57(9): 4578-4580.
9. Rawat D, Nair D. Extended-spectrum β-lactamases in Gram negative bacteria. J Global Infect Dis. 2010; 2(3): 263.
10. Shibl A, Al-Agamy M, Memish Z, Senok A, Khader SA, Assiri A. The emergence of OXA-48-and NDM-1-positive Klebsiella pneumoniae in Riyadh, Saudi Arabia. Int J Infect Dis. 2013; 17(12): e1130-e1133.
11. Lee C-R, Lee JH, Park KS, Kim YB, Jeong BC, Lee SH. Global dissemination of carbapenemase-producing Klebsiella pneumoniae: epidemiology, genetic context, treatment options, and detection methods. Front Microbiol. 2016; 7: 895.
12. Potron A, Poirel L, Rondinaud E, Nordmann P. Intercontinental spread of OXA-48 beta-lactamase-producing Enterobacteriaceae over a 11-year period, 2001 to 2011. Eurosurveillance. 2013; 18(31): 20549.
13. Fu Y, Du X, Ji J, Chen Y, Jiang Y, Yu Y. Epidemiological characteristics and genetic structure of bla NDM-1 in non-baumannii Acinetobacter spp. in China. J Antimicrob Chemother. 2012; 67(9): 2114-2122.
14. Yang J, Chen Y, Jia X, Luo Y, Song Q, Zhao W, et al. Dissemination and characterization of NDM-1-producing Acinetobacter pittii in an intensive care unit in China. Clin Microbiol Infect. 2012; 18(12): E506-E513.
15. Chen Y, Zhou Z, Jiang Y, Yu Y. Emergence of NDM-1-producing Acinetobacter baumannii in China. J Antimicrob Chemother. 2011; 66(6): 1255-1259.
16. Bogaerts P, Rezende de Castro R, Roisin S, Deplano A, Huang T-D, Hallin M, et al. Emergence of NDM-1-producing Acinetobacter baumannii in Belgium. J Antimicrob Chemother. 2012; 67(6): 1552-1553.
17. Bonnin R, Poirel L, Naas T, Pirs M, Seme K, Schrenzel J, et al. Dissemination of New Delhi metallo‐β‐lactamase‐1‐producing Acinetobacter baumannii in Europe. Clin Microbiol Infect. 2012; 18(9): E362-E365.
18. Boulanger A, Naas T, Fortineau N, Figueiredo S, Nordmann P. NDM-1-producing Acinetobacter baumannii from Algeria. Antimicrob Agents Chemother. 2012; 56(4): 2214-2215.
19. Poirel L, Bonnin RA, Boulanger A, Schrenzel J, Kaase M, Nordmann P. Tn125-related acquisition of blaNDM-like genes in Acinetobacter baumannii. Antimicrob Agents Chemother. 2012; 56(2): 1087-1089.
20. Hrabák J, Štolbová M, Študentová V, Fridrichová M, Chudáčková E, Zemlickova H. NDM-1 producing Acinetobacter baumannii isolated from a patient repatriated to the Czech Republic from Egypt, July 2011. Eurosurveillance. 2012; 17(7): 20085.
21. Espinal P, Fugazza G, Lopez Y, Kasma M, Lerman Y, Malhotra-Kumar S, et al. Dissemination of an NDM-2-producing Acinetobacter baumannii clone in an Israeli rehabilitation center. Antimicrob Agents Chemother. 2011; 55(11): 5396-5398.
22. Kaase M, Nordmann P, Wichelhaus TA, Gatermann SG, Bonnin RA, Poirel L. NDM-2 carbapenemase in Acinetobacter baumannii from Egypt. J Antimicrob Chemother. 2011; 66(6): 1260-1262.
23. Pfeifer Y, Wilharm G, Zander E, Wichelhaus TA, Göttig S, Hunfeld K-P, et al. Molecular characterization of bla NDM-1 in an Acinetobacter baumannii strain isolated in Germany in 2007. J Antimicrob Chemother. 2011; 66(9): 1998-2001.
24. Karthikeyan K, Thirunarayan M, Krishnan P. Coexistence of bla OXA-23 with bla NDM-1 and armA in clinical isolates of Acinetobacter baumannii from India. J Antimicrob Chemother. 2010; 65(10): 2253-2254.
25. Dortet L, Nordmann P, Poirel L. Association of the emerging carbapenemase NDM-1 with a bleomycin resistance protein in Enterobacteriaceae and Acinetobacter baumannii. Antimicrob Agents Chemother. 2012; 56(4): 1693-1697.
26. Mushtaq S, Irfan S, Sarma J, Doumith M, Pike R, Pitout J, et al. Phylogenetic diversity of Escherichia coli strains producing NDM-type carbapenemases. J Antimicrob Chemother. 2011; 66(9): 2002-2005.
27. Nielsen JB, Hansen F, Littauer P, Schønning K, Hammerum AM. An NDM-1-producing Escherichia coli obtained in Denmark has a genetic profile similar to an NDM-1-producing E. coli isolate from the UK. J Antimicrob Chemother. 2012; 67(8): 2049-2051.
28. Williamson DA, Sidjabat HE, Freeman JT, Roberts SA, Silvey A, Woodhouse R, et al. Identification and molecular characterisation of New Delhi metallo-β-lactamase-1 (NDM-1)-and NDM-6-producing Enterobacteriaceae from New Zealand hospitals. Int J Antimicrob Agents. 2012; 39(6): 529-533.
29. Peirano G, Ahmed-Bentley J, Woodford N, Pitout JD. New Delhi metallo-β-lactamase from traveler returning to Canada. Emerging Infect Dis. 2011; 17(2): 242.
30. Poirel L, Lagrutta E, Taylor P, Pham J, Nordmann P. Emergence of metallo-β-lactamase NDM-1-producing multidrug-resistant Escherichia coli in Australia. Antimicrob Agents Chemother. 2010; 54(11): 4914-4916.
31. Woodford N, Turton JF, Livermore DM. Multiresistant Gram-negative bacteria: the role of high-risk clones in the dissemination of antibiotic resistance. FEMS microbiology reviews. 2011;35(5):736-55.
32. Shaheen B. W., Nayak N., M. B. First reported case of New Delhi metallo (NDM) carbapenem-positive gene in Escherichia coli from companion animals in the United States. In Abstracts of the 52nd ICAAC, abstract C2–1219. San Francisco, CA. American Society for Microbiology. 2012.
33. https://www.ncbi.nlm.nih.gov
34. https://www.ebi.ac.uk
35. Singhal N, Kumar M, Kanaujia PK, Virdi JS. MALDI-TOF mass spectrometry: an emerging technology for microbial identification and diagnosis. Front Microbiol. 2015; 6: 791.
36. El-Malek FFA, Yousef AS, El-Assar SA. Hydrogel film loaded with new formula from manuka honey for treatment of chronic wound infections. J Global Antimicrob Resist. 2017; 11: 171-176.
37. www.facm.ucl.ac.be/intranet/CLSI/CLSI-2017-M100-S27.pdf.
38. Bidle KA, Kirkland PA, Nannen JL, Maupin-Furlow JA. Proteomic analysis of Haloferax volcanii reveals salinity-mediated regulation of the stress response protein PspA. Microbiology. 2008; 154(Pt 5): 1436.
39. Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009; 9(4): 228-236.
40. Miriagou V, Cornaglia G, Edelstein M, Galani I, Giske C, Gniadkowski M, et al. Acquired carbapenemases in Gram-negative bacterial pathogens: detection and surveillance issues. Clin Microbiol Infect. 2010; 16(2): 112-122.
41. FARMER III J. Enterobacteriaceae: introduction and identification. Manual of clinical microbiology. 2003.
42. Wang J, Li Y, Yan H, Duan J, Luo X, Feng X, et al. Semi-rational screening of the inhibitors and β-lactam antibiotics against the New Delhi metallo-β-lactamase 1 (NDM-1) producing E. coli. RSC Adv. 2018; 8(11): 5936-5944.
43. Djahmi N, Dunyach-Remy C, Pantel A, Dekhil M, Sotto A, Lavigne J-P. Epidemiology of carbapenemase-producing Enterobacteriaceae and Acinetobacter baumannii in Mediterranean countries. BioMed Res Int. 2014; 2014: 305784.
44. www.Phylogeny.fr.

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.